Why some people are naturally immune to HIV
With any virus, even devastating ones like Ebola and HIV, there are people who are exposed, often repeatedly, but somehow they never become infected or develop symptoms of disease. Though doctors have long wondered why, especially in the case of HIV, only today has a team of researchers found an explanation. Scientists at the University of Minnesota studying HIV-1 discovered some people have a specific variation of a gene, APOBEC3H, which produces an antiretroviral protein that inhibits the replication of HIV, Medical Daily reports.
“We have seven APOBEC3 genes within the variants of human population,” Dr. Reuben S. Harris, a professor in the department of Biochemistry, Molecular Biology and Biophysics, explained to Medical Daily. Of these seven genes, “only APOBEC3H varies within the human population,” Harris added. APOBEC3H itself has seven variations, and if you broadly group these into those that make stable and those that make unstable proteins, Harris told Medical Daily, “What we found is those that are stable confer resistance to some forms of HIV.”
This important finding may pave the way to new treatments and drugs.
Viral infectivity factor
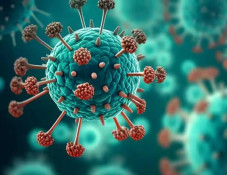
Viruses are often described as the ultimate parasite. They cannot reproduce or sustain themselves on their own, so they require a host. In the case of the human immunodeficiency virus, their host-of-choice is T lymphocyte cells found in the immune system. After gaining control of the molecular machinery of T-cells, the virus duplicates itself and then destroys its host. Naturally, this damages the immune system and so people infected with HIV become increasingly susceptible to any pathogen deciding to invade their bodies, including diseases like cancer.
However, this picture is somewhat simplistic. T lymphocytes possess their own defense mechanism in the form of antiretroviral proteins produced by the APOBEC3 genes. In turn, HIV has its own counter-defense — a protein referred to as viral infectivity factor (Vif), which tricks T lymphocytes into destroying APOBEC3 enzymes.
For the current study, then, a group of researchers led by Harris and doctoral student Eric Refsland decided to examine this interaction closely. They hypothesized that different levels of susceptibility to HIV-1 might be related to variations in the gene producing this antiretroviral protein.
Testing their theory, Harris and his colleagues first discovered that an HIV-1 infection increased APOBEC3H proteins. This, then, had to be an important part of the HIV susceptibility equation. Next, they “essentially took HIV strains,” Harris told Medical Daily, “And we figured out what amino acids are required to counteract APOBEC3H.” This was done by creating mutant probes to test how important a stable protein compared to an unstable protein might be when fighting off an HIV infection. “This is key,” Harris told Medical Daily. “If you can’t generate these mutants, it’s difficult to interpret the cell data.”
After creating the necessary probes, then, the research team used cells from donors and found different people with different genetic variations of APOBEC3H produced stronger and more stable antiretroviral proteins. The stable variations, the researchers found, successfully blocked HIV-1's ability to replicate itself in cases where the strain of HIV had a weak version of Vif.
Unfortunately, when the HIV-1 virus had a strong version of Vif, the protective proteins no matter how stable or potent lost their battle to infection.
Going forward, Harris says, he and his colleagues hope to learn ways to stop Vif from harming the APOBEC3 enzymes. "One could imagine drugs that stop Vif from binding with APOBEC," Harris said in a press release. Believing this to be “a bonafide HIV killing pathway,” Harris and his co-researchers want to activate it in infected persons. This approach might indefinitely suppress the virus and stop it from replicating, he speculates, or it could even result in curing HIV.
Newsfeed
Videos